The more complete and authoritative the diagnosis of prostatitis, the more effective the follow-up therapy. A doctor's formal approach can lead to long-term and ineffective treatment of the patient. Its job is to determine the inflammation of the prostate gland and all the factors that cause it.
How a doctor diagnoses prostatitis
Prostatitis is diagnosed by a urologist or male specialist. After talking with the patient, the doctor appoints the necessary tests: first standard collection (blood, urine, prostate secretions, rectal examination), then if indicatedusing high-tech, more detailed methods: CT, MRI, ultrasound.
Capture prehistory
During the initial consultation the doctor will ask the following questions:
- Intercourse time (if it becomes shorter, then under what circumstances);
- Presence of a sense of discomfort in the groin when in a stationary position for long periods of time, as well as after drinking alcohol or hypothermia;
- Frequency and rate of urination (are there any problems, are there interruptions, how often do you have to get up at night to go to the bathroom);
- Orgasm quality (still bright or dim, painful ejaculation).
The more details a patient remembers, the more complete the clinical image taken by the doctor.
Differential Diagnosis
The symptoms of prostatitis are similar to those of some other diseases:
- Cystitis (cramping when urinating, pain in the lower abdomen).
- Adenoma (difficult urination, heavy feeling in the groin).
- Prostate cancer (blood in urine, difficult urination).
- Rectal pathologies: hemorrhoids, adnexitis (inflammation), anal fissures, genital warts (ulcerative colitis).
Additional diagnostic methods and the reasons for using them are shown in Table 1.
Table 1. Differential diagnosis of prostatitis
| Disease | Risk group | Analyze |
|---|---|---|
| Increase production | Male over 45 years old with no history of urethritis, catheterization, bladder and urethral trauma (cases that can cause pain, blood in urine) | Ultrasound of the prostate gland and digital examination |
| Prostatitis | Mainly young male with recent fever and hypothermia, without a history of stimulating factors (like hyperplasia) | ultrasound, complete blood count (CBC), digital prostate exam |
| Prostate cancer | Male over 45 years old, no history of provoking factors | Prostate ultrasound, PSA analysis, digital examination |
If necessary, other specialists involved in the diagnosis: electrophologists, neurologists, spine specialists. Two specialists eventually determine the cause of the pain is related to a violation of the structure of the spine, infringement of the nerve ends.
Touch the rectum
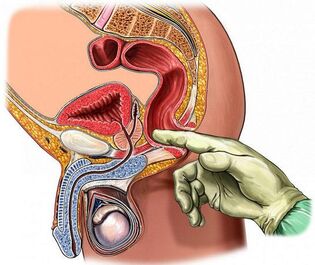
Digital rectal exam is the most accessible and most informative method of examining the condition of your prostate gland. During the surgery, the doctor pays attention to the following parameters about its structure:
- Volume;
- Density;
- Surface roughness;
- Homogeneity (tissue homogenization);
- Borders (border clarity);
- Preserves the isthmus (vertical stitches between lobes).
In prostatitis, enlarged glands due to edema (may not be asymmetric), consistency, elasticity, not palpable longitudinal grooves (sutures), pain when touching patients.
In order to have a clear picture for this type of diagnosis,preparation:
- Do not ejaculate the day before, do not drink alcohol, avoid strenuous exercise, hypothermia and overheating.
- Don't ride a bike for a day, don't use a rowing machine (don't injure or massage your prostate in this way).
- Before going to see a doctor, enema (a small enema may be used) to clean the rectal canal.
You can feel the prostate gland at a depth of 3-5 cm from the anus. The doctor performs the procedure using sterile gloves, lubricating the finger gel. Patient lies on his side, bends his knee or stands in a knee-elbow position.
Laboratory method
Laboratory methods for the diagnosis of prostatitis involve the study of biological materials for the presence of pathogens.
Blood
Based on the results of general and biochemical blood tests (taking capillaries from the finger), early prostatitis can be suspected. Analysis is done on an empty stomach in the morning. You should limit smoking for one hour before the procedure.
Important metrics:
- Leukocytes (blood cells, the number increases with a decrease in immunity against an inflammatory response). Usually 4-9 × 10 ^ 9 units;
- ESR (erythrocyte sedimentation rate). The norm is about 5 units, an increase indicates inflammation or a cancerous process;
- Lymph cells. Typically, the percentage of total blood cell volume ranges from 18 to 40 units. Excess means infection.
Men over 40 years of age indicated for PSA test- a tumor marker, exceeding this value means chronic prostatitis or prostate cancer.Norm- less than 4 ng / ml, after 50 years - 5. 33 ng / ml.
Urine
The urethra passes through the prostate gland (prostate of the urethra), so when the gland becomes inflamed, the urine changes color and viscosity. For the diagnosis of prostatitis, three types of analysis are performed:
- General - Defines physical and chemical parameters. Signs of an inflamed prostate: cloudy urine, white, alkaline, protein, white blood cells, pus, sometimes foam or blood. With prostatitis, phosphates are found.
- Cytology - checks the presence of pathologically altered cells. The presence of erythrocytes and epithelium may indicate a tumor process.
- Bacteriology - determine the activity of pathogenic microorganisms. To do this, make a sowing tank settle on nutrient medium. If there are bacteria and fungi, then over time they begin to actively multiply. Escherichia coli often causes prostatitis.
Before urinating, you should limit eating salty and spicy food, not drinking alcohol and coloring products (radish, coffee) Analysis was done in the morning on an empty stomach.For prostatitis, a three-cup test method is used:the patient has alternating bowel movements; The result is the first, middle, and last part. This method allows to determine the localization of the inflammatory foci: urethra, prostate gland, bladder. The four-cup method is more informative. Final urine samples are collected after prostate massaging for secretions.
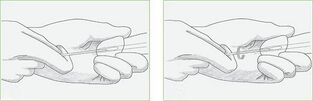
Prostate and sperm bile
Prostate translation is a valuable diagnostic agent. Preparing for his fence is the same as a rectal digital examination. To get enough bile, you should limit sexual intercourse for three to five days.
Method to check the secretion of the prostate gland:
- Microscope;
- Insert backward;
- PCR (polymerase chain reaction).
PCR is the most accurate method. For the treatment of biological materials, special enzymes are used to multiply the number of DNA and RNA fragments of the pathogen. The study requires a special device - amphlicator. The most accurate is real-time PCR. Results will be available in an hour.
Prostatitis is manifested by the presence in the juice of amyloid bodies, staphylococci, streptococci, Pseudomonas aeruginosa, epithelial cells (more than three units in the field of view). The number of lipoid particles decreased, and the number of white blood cells increased.
Anultrasound scan for prostatitis was an additional analysis. Against the background of prostatitis, sperm becomes yellow or brown, its viscosity increases (liquefies for a long time) and there are pathogenic microorganisms. In chronic prostatitis, epithelial cells of the gland, amyloid form and mucus are found.
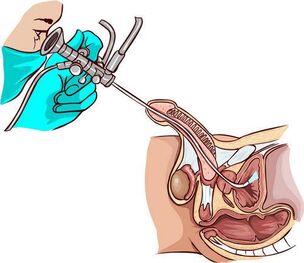
Urethral swab probe
Urethral gauze (curettage) is a less informative method for diagnosing prostatitis than analyzing the secretions.Used in the event that the following drug cannot be obtained due to hemorrhoids, exacerbation of inflammation, presence of calcification in the body of the prostate gland.
The process of taking this material out is quick but uncomfortable: the doctor dips a brush into the urethra to take out part of the cell that covers it along with microorganisms. The biological material is then examined by PCR, allowing you to determine the presence of pathogens in any quantity. The cause of prostatitis can be due to genital infections: chlamydia, Trichomonas, mycoplasma.
Before doing the analysis, you should refuse to have sex during the day, in the morning only perform external cleaning procedures for the penis (do not pour anything into the urethra), do not urinate for two hours.
Tool method
Diagnostic methodology tool allows you to confirm and supplement the results of laboratory tests.
Ultrasound and TRUS
Ultrasound exams of the prostate can help you visualize its structure, its outline, the nature of the tissue changes. In the case of prostatitis, transrectal ultrasound (TRUS) is considered to provide the best information: the doctor inserts a probe into the rectum. Prepare for the procedure in the same way as when palpation. Ultrasound of the abdomen (through the abdomen) is more comfortable for men, but the prostate gland cannot be seen completely due to the bladder.
With prostatitis, its structure is not uniform, the outline is blurred, the foci of fibrosis (overgrowth of connective tissue), scarring may be present. The prostate gland is enlarged, the groove between its lobes is smoothed.
MRI, PET and CT
If an ultrasound gives reasons to suspect the presence of a tumor, the doctor appoints a CT scan (computed tomography) or an MRI (magnetic resonance imaging) to clarify the image. The second type of study is more precise, but also more expensive. The procedures are painless, in terms of information content, they can replace a biopsy (removal of a piece of tissue).
CT and MRI show detailed structure of the prostate gland: stones, cysts, tumors, inflammatory foci, structural abnormalities. For a clearer picture, contrast is preliminarily injected into a vein (not for men with kidney failure). For the procedure, a suitable type of tomography and a rectal probe are used.
PET - CT of Positron emission. Allows you to analyze the condition of the prostate gland at the cellular and molecular level. It not only determines the presence and size of the tumor, but also determines the speed and quality of the metabolic processes that take place in it.
About the preparation:should empty the rectum. Do not eat for five hours prior to the procedure.
Features for diagnosing some types of prostatitis
Acute bacterial (infectious) prostatitis is diagnosed based on the patient's complaint, urine analysis, ultrasound, urethral smear. With active inflammation, the gland is sore, it is not allowed to intervene through the rectum, in severe cases, careful examination of the finger is required.
Laboratory data for the diagnosis of acute prostatitis are not very informative. Urine cultures may be recommended, but not required. With active inflammation, there is no time waiting for results. To relieve symptoms, antibacterial therapy with broad spectrum drugs is performed.
Chronic prostatitis practically does not manifest itself in any way, so to define it, it is necessary to have a wide range of laboratory, physical, instrumental methods. Determination of the patient's immune and neurological status may be required.
The palpation of the gland, urine and prostate secretions is paramount. The presence of more than 10 leukocytes in the field of view indicates inflammation. If the culture of the bacteria does not induce the growth of infectious microflora on the basis of the increased white blood cell count, then it is necessary to analyze for genital infections.
With a bacterial nature that causes inflammation, a large number of pathogens are found in the urine and prostate secretions. An undeniable microbiological sign of chronic inflammation: microbial count (CFU) more than 104 per ml. Some of them are numbered in the tens, so their presence in quantities between 10 and 102 per ml may indicate prostatitis.
In the case of bacterial (non-infectious) inflammation, they are not present, but experts recommend in these cases a further analysis should be done: prostate puncture, through which the pathogenlive in the extracted closed prostate glands. Simultaneously cultivate the sterile bacteria but ultimately find the pathogen. Usually, it is one of the types of E. coli bacteria.
Ultrasound does not always show chronic inflammation. In addition to the aforementioned methods, your doctor may prescribe ureter measurements - measuring the flow rate of urine with special sensors.
Typical comorbidities
For chronic chronic prostatitis with signs of colloid inflammation (tuberitis near the prostate gland),urethoscope - examination of tube imagewith endoscopic equipment. Helps determine narrowing of the urethra, a violation of its structure, the condition of the openings of the secretory canal of the prostate gland (mucus, pus, thickening) and tuberculosis.
Interpretation of the result (determine the stages of prostatitis according to the state of the tuberculosis):
- First: the seeds are red, edematous, bleeding. Similar patterns are observed in the back of the urethra;
- Second: cyclic increase and decrease in redness and swelling are characteristic;
- Third: skin changes in the tissues of the tuberculosis and urethra occur, so the lumen of the ureter may be narrowed (tightened).
Ureteroscopy stimulates the spermatozoa receptors, leading to impaired prostate microcirculation and motility, so the procedure is not unnecessarily performed.
Cystitis is also a companion of chronic prostatitis. Inflammation of the wall of the bladder was detected by ultrasound and cystoscopy. During the study, pathological changes in the mucous membranes are identified, especially in the neck area. The condition of the bladder against the background of chronic inflammatory prostate gland disease (hardening of the prostate gland):
- Triangular malformation of the bladder.
- The ureteral hole dilates.
- Narrow neck.
Cystoscopy is indicated at the end of the exam when lower abdominal pain is present and frequent urination.
The most difficult to diagnose is chronic bacterial prostatitis with unidentified pelvic pain. In such patients, doctors first of all conduct studies to rule out cystitis and neurological pathology.
How to diagnose prostatitis at home
A man can suspect acute prostatitis with the following signs:
- Severe pain in the lower abdomen and groin (between the testicles and anus);
- Body temperature increases;
- Pain when urinating (resembling cystitis);
- Premature and painful ejaculation.
The same symptoms appear during the exacerbation of chronic prostatitis, caused by hypothermia or heavy alcohol consumption. The development of this form of pathology can be demonstrated by periodic presence of blood in the urine, dull pain in the perineum (especially in a static position), difficulty urinating, impaired erection. Such signs are the reason to contact a urologist.
Conclusion
The longer the inflammatory process of the prostate gland is, the harder it will be to treat it, so you should not delay the diagnosis. In government agencies, most follow-up procedures and treatments are free.
























